Cystoscopy
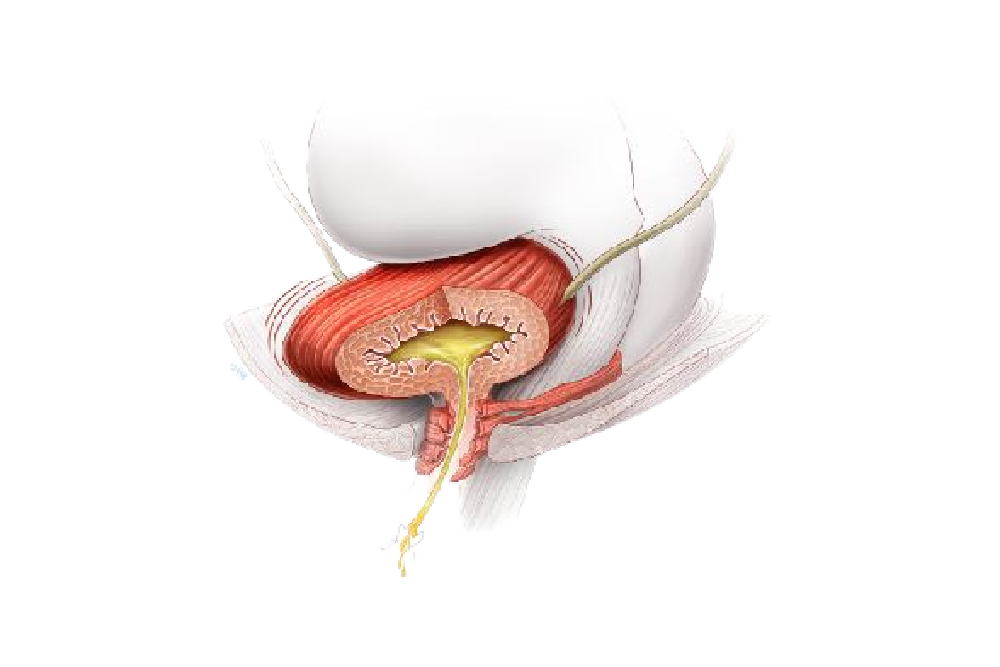
What is a cystoscopy? Cystoscopy is the name for a procedure allowing a doctor to look into your bladder and urethra with a special camera
Our clinic offers a wide variety of minimally invasive surgical options for female urology and urogynecology. Dr. Ingber and the staff at The Center for Specialized Women’s Health will work with you to ensure a seamless experience from start to finish. To learn more about surgical treatment, please call us at (973) 537-5557 to speak to a representative about your story.
What is a cystoscopy? Cystoscopy is the name for a procedure allowing a doctor to look into your bladder and urethra with a special camera

What is stress urinary incontinence (SUI)? SUI is a common problem affecting women which is caused by a weakness of the pelvic floor muscles (which

What is sacral nerve stimulation? Nerve stimulation is a reversible treatment for patients with bladder control problems in whom conservative treatments have not worked or

The purpose of the vaginal sling procedure is to create a hammock of support and to help prevent the urethra from opening when you cough,


What is genitourinary fistula? Genitourinary fistulas are abnormal passages or openings between the vagina, urethra, bladder or ureter. This abnormal passage may occur between the
Botulinum Toxin (BOTOX) for the Bladder Introduction Botox is currently FDA-approved for the treatment of overactive bladder (OAB) and neurogenic detrusor overactivity (NDO). Proper bladder

Introduction Vaginal prolapse is a common condition causing symptoms such as a sensation of bulging, fullness or pressure in the vagina; difficulty emptying the bowel

Vaginal and Uterine Suspension Procedures Over 120,000+ cases of uterine and vaginal vault prolapse are surgically treated each year in the U.S. Prolapse(or falling) of

Over 120,000+ cases of uterine and vaginal vault prolapse are surgically treated each year in the U.S. Prolapse (or falling) of any pelvic floor organ

What is posterior vaginal wall prolapse? About 1 in 10 women require surgery for vaginal prolapse. A prolapse of the back (posterior) wall of the

Hysterectomies are routine gynecological procedures used to remove a woman’s uterus and sometimes her ovaries and fallopian tubes as well. When the uterus is removed,

What is surgical mesh? Surgical mesh is a screen-like material that is used as a reinforcement for tissue or bone. It can be made of

What is a urethral diverticulum? A urethral diverticula is described as a cystic structure that is adjacent to the urethra. It is thought to arise

Vasectomy is a simple, safe, and effective means of permanent birth control or sterility. Each year about one-half million men in the United States are

Introduction Prolapse of the vagina or uterus is a common condition with 11-19% of women undergoing surgery for prolapse during their lifetime. Prolapse often occurs

What are the labia? There are two parts to the labia. The labia minora, also known as the inner lips, consist of 2 flaps of
When you awake after surgery, you may have a catheter (a tube) that drains urine from the bladder into a bag, and/or have a gauze pack placed in your vagina to prevent bleeding. Your doctor will specify how long these will need to stay in place based on your individual situation (usually between 8-24 hours).
The risk of developing a deep vein thrombosis (clots in the veins in the legs) increases when you are not active for a long period of time, such as during and following surgery. To minimize this risk, you may have special devices on your lower legs during surgery that regularly squeeze your legs to help reduce the risk of developing blood clots in your legs or lungs. You may also receive an injection of blood thinner medication and may be prescribed compression stockings to wear on your lower legs. While you are in bed, try to do simple exercises such as moving your ankles briskly in a circular motion, and bending and straightening your legs a few times each hour. Avoid crossing your legs. The best way to prevent blood clots from forming in your legs/lungs after surgery is to be up and out of bed as soon as possible after surgery. Try to take 3-4 short walks daily.
Following this major surgery, you can expect to experience some pain or discomfort in the groin, vagina, and lower abdomen. If you have had a sacrospinous suspension (vaginal vault or uterine) you may also experience a sharp or aching pain deep in your buttock(s). Pain should gradually decrease every week. It will take several weeks for the pain to go away completely. You will be given pain medication to help keep you comfortable. This means you will have less pain after you take the medication, but you will still have some pain. You should not expect the medication to get rid of all the pain. Painkillers will be prescribed after discharge, but often over-the-counter medication is sufficient. Pain relief should be taken at regular intervals. Do not wait for the pain to become too severe before taking medication. If you are experiencing severe pain that does not change at all after taking pain medication, contact your doctor.
Your doctor may advise additional preventive measures based upon your individual risk of developing a blood clot.
About 5-10% of women have difficulty emptying their bladder fully after surgery. This may be due to swelling or other causes that usually go away in a few days to 2 weeks. Since the bladder still needs to be emptied during this recovery time, you will either have a catheter or you will be taught how to catheterize yourself during this time (see Intermittent Self Catheterization leaflet). You may also notice that your urine flow is slower or different from before surgery. It may take longer than normal to empty your bladder than it did before surgery.
Constipation is a common problem following surgery. It is important to avoid excessive straining to pass a bowel motion as this will put pressure on the stitches in your vagina. Try to eat plenty of fruit and fiber and drink plenty of fluids to keep your stool soft after surgery. Stool softeners and/or laxatives are often prescribed after surgery to help prevent constipation. Take these as advised by your doctor. Some women experience burning or shooting pains in the rectum after surgery. This usually decreases within a few days after surgery.
It is normal to have some vaginal bleeding after surgery. At first the blood might be bright red. Later this usually changes to a darker reddish brown. The amount of bleeding can vary from day to day. You may also notice a little more bleeding after you walk. This is also normal. The bleeding will decrease over the weeks following surgery. If you experience heavy fresh red bleeding or clots requiring frequent pad changes, contact your doctor.
As the bleeding decreases, you may notice a creamy white discharge that may last for about another 8 weeks. This discharge is due to the stitches in the vagina dissolving.
Do not use tampons for the first 6 weeks after surgery. Use pads.
You can shower as soon as you feel up to it. Many people shower the day after surgery. Avoid prolonged soaking of the surgical area. Showering is preferable to bathing in the first 6 weeks after surgery when vaginal stitches are still present.
You can eat and drink as usual as soon as your appetite returns after the operation. You can eat any foods you desire, however, aim for nutritious foods that will help your body heal. Try to eat foods high in protein and fiber. Drink plenty of water to keep your stool soft (about 65 oz or 2 liters).
It is recommended to discontinue all use of tobacco products before surgery, and to not resume its use after surgery. Nicotine increases the risk of wound infection and may result in your wound healing more slowly or incorrectly.
Walking is a good form of activity as it puts little strain on your surgical repair, exercises your lungs, and can prevent deep vein thrombosis. Walk at a comfortable pace. Start by walking outside your hospital room the day after surgery. After you are discharged from the hospital, continue to take daily walks around your home or neighborhood.
It is usually safe to start pelvic floor exercises when you feel ready, usually 1 to 2 weeks after surgery. Discuss this with your doctor.
Do not try to exercise to gain fitness for at least 6 weeks after surgery. Avoid carrying or lifting more than 20 pounds or 9 kilograms (i.e. children, heavy bags, etc.) and avoid high impact exercise (i.e. running, gym training, weightlifting, horseback riding, etc.). These activities put pressure on the surgical repair before it has fully healed. This can prevent proper healing and increase the risk of having a recurrence of the prolapse.
Avoid vaginal intercourse or placing anything in the vagina for at least 6 weeks after surgery. The stitches in the vagina can be damaged if you insert anything in the vagina during this time. Your doctor will evaluate you at your post-operative visit and tell you if/when it is safe to resume vaginal intercourse. When you do resume vaginal intercourse, it may be a little uncomfortable to begin with, so take things slowly and gently. Vaginal lubricant use is encouraged. If intercourse remains uncomfortable after 3-4 months of regular intercourse, seek advice from your doctor.
You should not drive if you are taking sedative painkillers or are not confident that you could perform an emergency stop if needed. As a general guide, avoid driving for 1 to 2 weeks. If you are unsure, check with your doctor. Some insurance companies place restrictions on driving after surgery, so check your policy details.
Most patients return to work after about 6 weeks. This varies and depends on your surgery, recovery, and the type of work you do. It may be advisable to try to organize a shortened work week or light duties when you first return to work, especially if your job involves prolonged standing or heavy lifting. Your medical team will discuss this with you.
Everyone recovers at a different rate. This depends on several factors: your health and fitness level before surgery, whether complications occurred during or after surgery, and the type of surgery performed. It is important to listen to your body and take time to rest. Do not try to push yourself too hard. Over the course of 4-6 weeks your body will gradually heal, and your energy level will slowly rise to your normal level.
If you develop heavy bleeding or a foul-smelling vaginal discharge, burning or stinging on passing urine, increasing abdominal pains, vomiting, fever, painful swollen leg(s), shortness of breath or chest pain, seek medical advice