Vaginal and Uterine Suspension Procedures
Over 120,000+ cases of uterine and vaginal vault prolapse are surgically treated each year in the U.S. Prolapse(or falling) of any pelvic floor organ (vagina, uterus, bladder or rectum) occurs when the connective tissues or muscles within the body cavity are weak and unable to hold the pelvis in its natural orientation.
The weakening of connective tissues accelerates with age, after child birth, with weight gain and strenuous physical labor. Women experiencing pelvic organ prolapse typically have problems with pelvic and vaginal pressure, urinary incontinence, vaginal ulceration, sexual dysfunction and/or having a bowel movement.
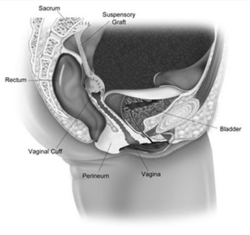
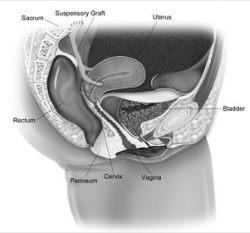
Sacral colpopexy and hysteropexy
Sacral colpopexy is a procedure to surgically correct vaginal prolapse where mesh is used to hold the vagina in the correct anatomical position. This procedure may be performed several years after a hysterectomy, or, at the same setting as a hysterectomy. Alternatively, for women with a possibility of future pregnancy, or for women who desire uterine-sparing approaches, a hysteropexy can be performed. This involves placement of mesh on the vaginal wall and cervix from the inside. The mesh is then secured to a strong ligament within the pelvis.
In the past, these surgeries were performed as an open surgery. A 15-30 cm incision was made in the lower abdomen in order to manually access the inter-abdominal organs, including the uterus.
da Vinci® Sacrocolpopexy or Sacral Hysteropexy
This procedure uses a state-of-the-art surgical system designed to help your surgeon perform a minimally invasive surgery through 5 to 6 small incisions. Special instruments are inserted through these incisions, and the surgeon sits at a console (control center) adjacent to the patient in the operating room. The surgeon controls each instrument through the console, and an assistant is present at the side of the patient.
Laparoscopic and Laparoendoscopic Single-Site (LESS) Sacral Colpopexy and Sacral Hysteropexy
Laparoscopic approaches use 3 to 4 small incisions. A camera is inserted and special instruments are used by the surgeon to perform the procedure. With LESS procedures, only one incision is made, typically near the umbilicus (belly-button). Special flexible instruments are inserted through this incision and are used to perform the surgery. Because the incision is made only in a natural orifice such as the belly-button, the scars are often hidden.
What do these surgeries entail?
Vaginal and uterine suspension procedures are either performed on an outpatient basis, or typically with a stay of 23 hours in the hospital or in an ambulatory surgical center. Occasionally we perform concomitant hysterectomy at the time of suspension if a uterus is still in place. Since these procedures involve only small incisions with minimal dissection, there is less discomfort and more rapid healing. Typically, a permanent mesh material, made out of polypropylene is secured to the falling organ and secured to a strong ligament within the pelvis. Occasionally, an additional vaginal procedure may be required to tighten the muscles under the bladder or rectum (cystocele/rectocele repair). Often times, a vaginal sling is placed at the time of surgery in order to prevent stress incontinence in the future.

What are the risks and complications of sacral colpopexy and hysteropexy?
Complications of this type of procedure are rare but may occur. The most common complications include bleeding and infection, erosion or infection of the graft material (possibly requiring further surgery), injury to nearby structures, pain, inability to urinate (retention of urine), recurrent or worsening incontinence, new or worse vaginal prolapse, urgency or urge type-incontinence.
What happens after surgery?
Following your surgery, your vagina may be packed for a short time with a gauze roll to act as a bandage to prevent bleeding. You may have a catheter exiting from the urethra or from a small incision above the hairline (called a suprapubic tube or “SP”) for a short period of time. In most cases, patients go home without a catheter, as most patients void in the recovery area. The catheter is in place to allow you to empty your bladder, as there is often swelling after surgery that prevents you from being able to urinate. After the swelling subsides you will gradually be able to urinate. The normal pattern of urination may not occur for a few weeks so there is no cause for alarm. You can resume a normal diet but should limit your fluids to no more than 6 glasses per day. You will be discharged home with narcotic pain medicines. Every patient’s pain tolerance is different; some do not require any narcotics after surgery, while others require several days’ worth. We typically recommend stool softeners which can be purchased over the counter.
You should not lift anything heavy (more than 5 to 10lbs) for 4-6 weeks following these procedures. Additionally, you should refrain from sexual activity for 4-6 weeks. Your doctor will instruct you when it is safe to resume your usual activities.


