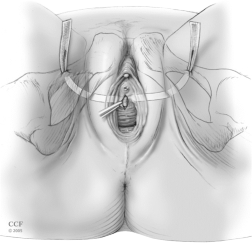
The purpose of the vaginal sling procedure is to create a hammock of support and to help prevent the urethra from opening when you cough, sneeze, or laugh. The procedure involves placing a piece of material under the urethra. The material options available to us include synthetic material, your own tissues, or other selective tissue sources. The procedure can be performed in one of two ways: just above the vagina on the lower abdomen (retropubic) or into the groin creases (transobturator technique).
Many patients also have a cystocele (dropped bladder), rectocele (herniated rectum into the vagina), uterine, or small bowel (enterocele) prolapse. If so, we may need to broaden the scope of your surgery and may use mesh to help in the repair. Your own tissues will typically become incorporated into the mesh in a few months. If your own tissues appear too weak, we may recommend the use of other tissues or materials to help our repair. The materials we use include cadaveric tissue, porcine tissue or synthetic materials to provide additional support to the bladder and urethra.
What does the surgery entail?
Vaginal sling procedures are usually performed on an outpatient basis in the hospital or in an ambulatory surgical center. The procedures are done entirely through through the vagina. A small incision may be necessary just above the hairline or in the thigh creases for placement of some sutures or the sling. Since this is only a small incision with minimal dissection, there is less discomfort and more rapid healing. You will have absorbable sutures in the vagina that dissolve in several weeks time.
What are the risks and complications of the vaginal sling procedure?
Complications of this type of procedure are rare but may occur. The most common complications include bleeding and infection, erosion or infection of the graft material (possibly requiring further surgery), injury to nearby structures, pain, inability to urinate (retention of urine), recurrent or worsening incontinence, new or worse vaginal prolapse, urgency or urge type-incontinence.
What happens after surgery?
Following your surgery, your vagina may be packed for a short time with a gauze roll to act as a bandage to prevent bleeding. In most cases, patients go home without a catheter, as most patients void in the recovery area. If you have a suprapubic tube, it will be capped prior to your discharge. The catheters are in place to allow you to empty your bladder, as there is often swelling after surgery that prevents you from being able to urinate. After the swelling subsides you will gradually be able to urinate. The normal pattern of urination may not occur for a few weeks so there is no cause for alarm. You can resume a normal diet but should limit your fluids to no more than 6 glasses per day.


